Among
patients who have recovered from COVID-19 in China comes the first evidence
that some may suffer long-term lung damage from the disease.
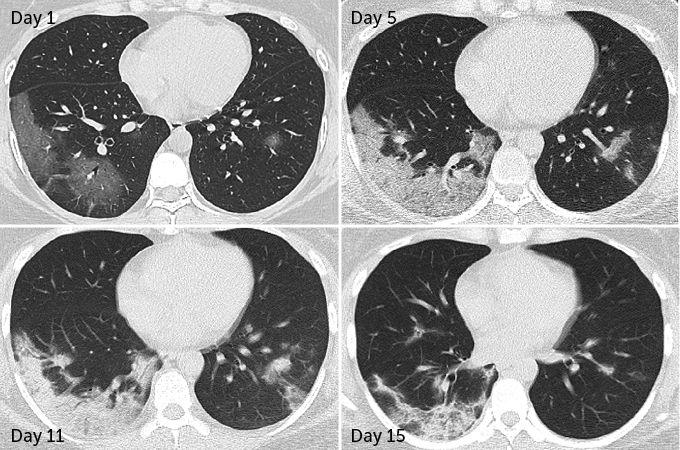
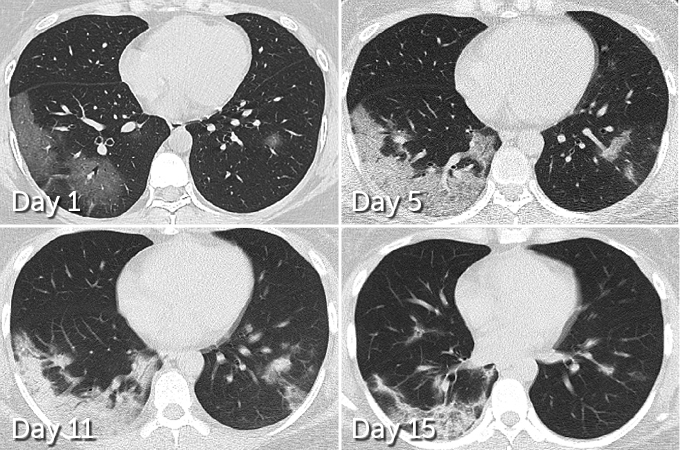
In 70
patients who survived COVID-19 pneumonia, 66 had some level of lung damage visible in CT scans taken before
hospital discharge, researchers report March 19 in Radiology. The damage ranged from dense clumps of hardened tissue
blocking blood vessels within the tiny air sacs called alveoli, which absorb
oxygen, to tissue lesions around the alveoli, Yuhui Wang, a radiologist at
Huazhong University of Science and Technology in Wuhan, China, and colleagues
found.
The tissue lesions can be a sign of chronic lung disease. Similar
damage has been documented in survivors of SARS and MERS, respiratory diseases caused
by coronaviruses similar to the SARS-CoV-2 virus behind COVID-19. Long-term
studies of SARS patients have shown that roughly a third of people who
recovered from severe bouts were left with permanent lung damage. In the case
of MERS, one study found about a third of people who recovered from a serious
infection still had signs of lung damage about seven months later.
But while initial lung images indicate that SARS and MARS
typically set into just one lung, COVID-19 appears to be more likely to afflict
both lungs right away. In 75 of the 90 patients
admitted to Huazhong University Hospital with COVID-19 pneumonia from January
16 to February 17, damage was seen across both lungs, Wang and colleagues
report. CT scans taken before hospital discharge revealed that 42 out of 70 patients
displayed the type of lesions around the alveoli that are more likely to
develop into scars.
Given how widely the pandemic has spread, chronic lung
conditions from COVID-19 could challenge many thousands of people in years to
come. As
of April 27, more than 2.9 million people worldwide have been diagnosed with
the disease. In
comparison, SARS, or severe acute respiratory syndrome, sickened about
8,000 people during its 2003–2004 outbreak. MERS, or Middle East
respiratory syndrome, has infected more than 2,500 people (SN: 1/24/20). While an estimated 80 percent of COVID-19 cases are
mild, the rest display problems
ranging from breathing difficulties to respiratory failure (SN: 2/25/20).
Some lung damage seen in the Wuhan study cases are likely to
gradually heal or disappear, Wang and colleagues suspect. However, in some
patients, lung abnormalities will harden into layers of scar tissue known as
pulmonary fibrosis. That scarring stiffens the lungs, making it hard to get
enough oxygen. People with pulmonary fibrosis typically suffer shortness of
breath, limiting their ability to be physically active.
Certain patients are most at risk of developing this type of
scarring. They include elderly patients who’ve had severe bouts of COVID-19 pneumonia,
patients with other illnesses such as cancer or diabetes and those with other lung
conditions caused by smoking or pollution, says Xiaolong Qi of the First
Hospital of Lanzhou University in China, where another COVID-19 lung damage
study is under way.
A hyperactive
immune response may be to blame for scarring.
A sudden storm of molecules called cytokines causes inflammation that can
damage lung tissue and fill the alveoli with pus. In the worst cases, damage
from this inflammation is so severe that it eventually leaves thickened scar
tissue in honeycomb-shaped clusters — something also seen in SARS and MERS.
While it’s unclear whether any of the Wuhan patients had such severe damage,
it’s been
described in other COVID-19 cases.
Breathing with the help of a ventilator can also cause lung
damage, and it may be difficult to tell which patients’ injuries stem from a
dysfunctional immune response to the virus versus being on ventilator, says radiologist
Karuna Das of United Arab Emirates University in Al Ain. Having studied MERS
patients, Das is now investigating the long-term health impact of COVID-19.
“During the MERS outbreak, some patients were on ventilators
for more than 100 days,” he says. “Oxygen is being infused with positive
pressure, and when the lungs get inflated beyond their limits, it causes
trauma.” About
a third of MERS patients who suffered lung damage had not fully recovered
more than seven months on, Das and colleagues reported in 2017 in the Indian Journal of Radiology and Imaging.
Long-term outcomes for SARS survivors also suggest some
COVID-19 patients may face lasting lung problems. Researchers at a Beijing
hospital found that the
percentage of lung lesions across 71 patients changed little between 2004
and 2018, as reported February 14 in Bone
Research.
“Based on what we have seen from SARS, MERS and H1N1 influenza, we expect that at least some COVID-19 patients will have some residual disease,” says Ali Gholamrezanezhad, a radiologist at the University of Southern California in Los Angeles. He and coauthors review lessons from SARS and MERS in the May American Journal of Roentgenology. Some survivors, he says, will have “some residual fibrosis, scars and their lung function and their lung anatomy doesn’t go back to normal.”










